Benefits Investigation and Prior Authorization
At HNL Lab Medicine, we take the complexity out of billing so that you can focus on what matters most; your patients’ health.
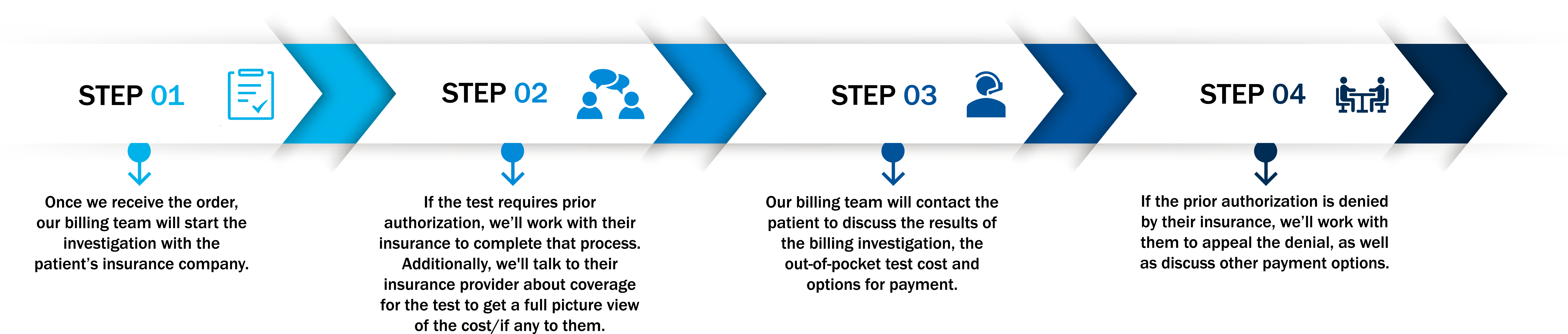
When your provider orders a test, we’ll check with your patient’s insurance provider to make sure the test is covered and give them a full picture of what their out-of-pocket cost may be.
Prior Authorizations
Many third-party payers require prior authorization for patients in need of important genetic and molecular laboratory testing. Without a prior authorization, your patient’s claim for reimbursement of the test will be rejected and they may receive a significant bill.
In order to reduce your workload, HNL Lab Medicine will submit a prior authorization request on behalf of you and your patient so that testing can be authorized, performed and reimbursed without significant delay or co-payment required.
The prior authorization process requires that the insurance company is provided necessary clinical information to support the clinical need for the test. In order to simplify the process, you can utilize this prior authorization packet to easily collect the relevant information that we may convey to the insurance company. If we need additional information, an HNL Lab Medicine representative will reach out to your office.
HNL Lab Medicine will process the patient’s specimen to ensure stability of the specimen but may hold the specimen and not complete the test until all information for the prior authorization is received.

Prior Authorization, also known as a pre-authorization or pre-certification, is a clause in the health insurance policy that says the patient must get permission from their health insurance company before they receive certain health care services which includes specialized laboratory testing. This process was developed to help ordering health care professionals, laboratories, and their patients receive a quicker coverage determination by giving them information:
- If a member’s benefit plan requires prior authorization.
- When additional clinical information is required to make a coverage decision.
- Whether the request meets third party’s clinical and coverage policy criteria.
The health care professional who is ordering the testing is responsible for obtaining prior authorization for the specialized laboratory test. If the health care professional’s office does not obtain the necessary prior authorization before testing, the patient will be responsible for payment, which can range in cost from just under one hundred dollars to thousands of dollars based on the test ordered.
Yes! If you complete the Clinical History Form, we can attempt the process for you.
If prior authorization is denied, the ordering facility will be notified and given the option to cancel the test. If the test is canceled, a DNA extraction fee may apply.
Our experts would be happy to assist you with all questions regarding prior authorization. For billing related questions contact 844-HNL-BILL. For all clinical related questions, please contact HNL Genomics (CTGT) via 484-244-2900.
Clinical coverage reviews will be based on third party clinical policy requirements for coverage. These policies include clinical criteria and information about coverage eligibility for related services. If a request needs review or requires additional clinical information, we will contact the ordering health care professional.
Specialized laboratory testing that requires prior authorization can usually be found on the health plan’s website or by calling the health plan directly. Many genetic and molecular tests require prior authorization for outpatient services.
Prior Authorization for genetic and molecular laboratory testing is required by many, but not all, third party payers.
HNL Lab Medicine will process and hold all specimens referred for genetic and molecular laboratory testing until all necessary clinical information for prior authorization submissions are received. For all other testing, specimens will not be held.
HNL Lab Medicine reserves the right to bill the client or your patient for genetic and molecular laboratory testing in which prior authorization information is not received, or the third-party payor denies the request.
Prior Authorization is not a guarantee of payment. In some circumstances, even after the insurance approved the prior authorization, they still refuse the payment. When this happens, HNL Lab Medicine will work with the insurance company to appeal the denial.